Topic 14 Fluid and electrolytes imbalance procedures:
TOPIC 14
Fluid and electrolytes imbalance procedures:
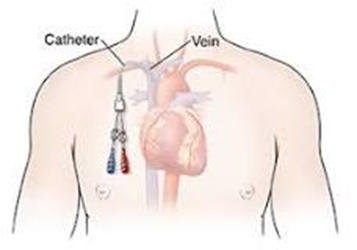
• Prepare and assist in setting up of Central Venous Line (CVL)
• Perform Central Venous Pressure reading Output
Introduction
Many healthcare practitioners inserts central lines. Central line placement is essential in caring for many critically ill and hospitalized patients. Like any procedure, it has its complications, some of which can be life-threatening. Complications of central line placement include pneumothorax, hematoma, bleeding, infection, and extravasation. Understanding this procedure's proper technique and potential complications can help minimize central line-associated complications and improve clinical outcomes. This activity reviews the indications, techniques, possible complications, and ways to reduce the risk of complications associated with central line placement to increase healthcare provider knowledge and ability of the procedure and improve clinical outcomes.
With ultrasound guidance, standardized techniques, new catheter designs, and central line care bundle, this procedure has become ubiquitous in the intensive care unit.
LEARNING OUTCOME
At the
end of the lecture, the students will be able to:
1.Demonstrate the ability to reflect upoun nursing practice for awareness and
improvement
2. Identify the importance of each procedures that would lead early and late complications.
Indications for placing a CVL include the following:
Drug infusions that could otherwise cause phlebitis or sclerosis (e.g., vasopressors and hyperosmolar solutions)
Monitoring
Central venous pressure
Central venous oxyhemoglobin saturation (ScvO2)
Pulmonary artery pressure
Emergency venous access (due to difficult peripheral intravenous access)
Transvenous pacing wire placement
High-volume/flow procedures requiring large-bore access (haemodialysis and plasmapheresis)
Vena cava filter placement
Venous thrombolytic therapy
What are 5 indications for central lines?
Indications for central venous access via the subclavian approach to the subclavian vein include the following:
Volume resuscitation.
Emergency venous access.
Nutritional support.
Administration of caustic medications (eg, vasopressors)
CVP monitoring.
Transvenous pacing wire introduction.
Haemodialysis
Complications of CVL placements include arterial puncture, catheter malposition, pneumothorax, subcutaneous hematoma, hemothorax, and cardiac arrest (exceedingly rare). The use of real-time ultrasound guidance can significantly decrease the complication rates of this procedure
Periprocedural Complications
Pneumothorax is a severe complication of subclavian and internal jugular vein catheter placements. However, the internal jugular approach is associated with a lower rate of pneumothorax
. Venous air embolism, though potentially fatal, is an infrequent complication of this procedure and can be minimized by correctly positioning the patient and using diaphragms that prevent significant air embolism.
Arterial puncture and injury are severe complications of this procedure, and every effort should be made to avoid their occurrence. As stated above, consistent use of real-time ultrasonography can prevent this complication.
If arterial trauma and cannulation occur, endovascular treatment is the best approach to minimize hematoma, airway obstruction, stroke, and false aneurysm
If inadvertent arterial cannulation with a catheter occurs, it is better to leave the catheter in place and attempt treatment with a percutaneous closure device.
Ventricular arrhythmias are known complications of this procedure and are related to the placement of the guidewire and catheter tip beyond the Cavo atrial junction Careful monitoring of the guidewire length as it is advanced into the vessel and determining adequate catheter length before securing it can avoid this potentially lethal complication.
Late Complications
Catheter-related bloodstream infections (CR-BSI) are well-recognized complications of this procedure and are associated with increased morbidity and mortality for the patient The most critical risk factor for these infections is a longer duration of use, especially in dialysis patients Sequalae of CR-BSI include metastatic infections to vertebral bone or disc space, endocarditis, and endovascular infections.
Central vein stenosis is another late complication of this procedure and is most prominent in chronic haemodialysis patients who often undergo repeated cannulations of the central veins. The highest risk of this complication occurs in the left-sided internal jugular or subclavian vein cannulations. Other risk factors include using haemodialysis catheters instead of flexible triple-lumen catheters and a longer duration of catheter-dwelling time.
In addition to central venous stenosis, catheter-related deep vein thrombosis (DVT) can also occur. Catheter-related DVT is most common in patients with underlying malignancy and using peripherally inserted multi-lumen catheters. The below-mentioned table summarizes the early and late complications associated with central venous line placement.
|
Complications Associated with Central Venous Placement |
|
|
Early |
Bleeding Arterial puncture Arrhythmia Air embolism Thoracic duct injury Mispositioning of catheter Pneumothorax Haemothorax |
|
Late |
Infection Venous thrombosis Central vein stenosis Pulmonary embolism Venous stasis Catheter malfunction Catheter migration Catheter perforation Nerve injury |
Healthcare Team Outcomes
This requires an interprofessional team of clinicians and nurses. The critical care nurse must perform daily dressing inspections, periodically change the dressing following strict aseptic technique to prevent catheter-related infections, and report back to the clinician managing the case if any concerns arise, so corrective action(s) can be taken. An aseptic technique is also required when accessing the ports of the CVL.
Depending on the line's location, complications like pneumothorax, hematoma, bleeding, or extravasation can occur and should be monitored. Healthcare workers should generally avoid lines in the groin for more than 24 to 48 hours as they are prone to infections and make it difficult for the patient to ambulate or get out of bed. To ensure good practice and limit complications, most hospitals now have an interprofessional team of healthcare professionals in charge of central line insertion and monitoring, each checking and communicating any issues noted to the rest of the team so corrective action can occur if necessary. This universal practice has been shown to limit complications and optimize clinical outcomes for patients undergoing this procedure In the event of an infection, an infectious disease specialty pharmacist may be consulted to best target antimicrobial therapy.
What are the problems with central venous line?
Complications included failure to place the catheter (22 percent), arterial puncture (5 percent), catheter malposition (4 percent), pneumothorax (1 percent), subcutaneous hematoma (1 percent), hemothorax (less than 1 percent), and cardiac arrest (less than 1
What are signs of CVC problems?
If you notice any of these signs of infection, tell your doctor or nurse right away:
Signs of infection, clotting, or other problems include:
Redness, tenderness, drainage, warmth, or odor around the catheter site.
Fever of 100.5F (38 C) or greater, or chills.
Swelling of the face, neck, chest, or arm on the side where your catheter is inserted.
Leakage of blood or fluid at the catheter site or the cap
Yellow or green drainage.
Pain or discomfort
· What is the most common cause of central catheter infection?
Approximately 40%–80% of CRBSIs are caused by gram-positive organisms. Coagulase-negative Staphylococci, Staphylococcus aureus, and Enterococcus are the most common organisms. Methicillin-resistant staphylococcus is frequently seen
What is the responsibility of central line nurses?
Central Line Nursing is the insertion, care, and maintenance of Central Line Catheters by trained nurses. Highly skilled nurse specialists typically will place the Central Lines, lines that end in a large vein above or below the heart, and other nurses will be responsible for the care and maintenance of the lines
How do you care and maintain central lines?
Preventing a Problem with a Central Line
Wash your hands before doing any central line care and wear gloves.
Always keep a clean and dry dressing over the central line site.
· Follow the instructions for cleaning the cap and using sterile equipment.
Avoid tugs or pulls on the central line
What instructions should you give a patient who has a central line?
Keep the central line dry. The catheter and dressing must stay dry. Don't take baths, go swimming, use a hot tub, or do other activities that could get the central line wet. Take a sponge bath to avoid getting the central line wet, unless your healthcare provider tells you otherwise.
Why is it important to flush a central line?
A CVAD should be flushed as often as your doctor tells you, to keep it clear of blood and prevent clotting. If it ends in more than one line (lumen), flush them in the same order each time. Depending on the type you have, you will flush it with either heparin or saline solution
How do you ensure accuracy of CVP reading?
To ensure accurate central venous pressure (CVP) readings, make sure that the manometer base is aligned with the patient's right atrium (the zero-reference point). The manometer set usually contains a leveling rod to allow you to determine this alignment quickly.
What happens if CVP is high?
Elevated CVP will present clinically as a pulsation of the internal jugular vein when a patient is inclined at 45 degrees; however, it can be noted in an upright patient in severe cases. Elevated CVP is indicative of myocardial contractile dysfunction and/or fluid retention
· What happens if CVP is low?
· Low CVP can occur with hypovolemia or a fall in effective circulating volume, as occurs with distributive shock. Cardiogenic shock (or fluid overload) can result in an elevated CVP, because forward failure of the cardiac pump results in backup of blood within the venous side of the system
Clinical pearls for consideration:
· A chest X-ray should be performed immediately for the internal jugular and subclavian lines to ensure proper placement and the absence of an iatrogenic pneumothorax.
Be sure you withdraw venous blood before dilation and cannulation of the vessel.
Never force the guidewire on insertion because it may cause damage to the vessel or surrounding structures. Forcing the wire could also cause it to kink, making removal difficult and causing damage to the vessel wall. It may also lead to an inaccurate position of the catheter.
· Always place your finger over the open hub of the needle to prevent an air embolism.
Always confirm placement with ultrasound, looking for reverberation artefact of the needle and tenting of the vessel wall. Needles cannot be visualized on ultrasound. Wires can be visualized so the operator can also confirm at that step.
A venous blood gas can be aspirated off a femoral line to ensure it is not arterialEnhancing Healthcare Team Outcomes
Central line placement is a common, often bedside, procedure. Placement under strict sterile conditions and subsequent catheter management, as well as a daily review of the need for continuing the central catheter, can help minimize complications associated with this procedure. This requires an interprofessional team of clinicians and nurses. The critical care nurse must perform daily dressing inspections, periodically change the dressing following strict aseptic technique to prevent catheter-related infections, and report back to the clinician managing the case if any concerns arise, so corrective action(s) can be taken. An aseptic technique is also required when accessing the ports of the CVL.
Depending on the line's location, complications like pneumothorax, hematoma, bleeding, or extravasation can occur and should be monitored. Healthcare workers should generally avoid lines in the groin for more than 24 to 48 hours as they are prone to infections and make it difficult for the patient to ambulate or get out of bed. To ensure good practice and limit complications, most hospitals now have an interprofessional team of healthcare professionals in charge of central line insertion and monitoring, each checking and communicating any issues noted to the rest of the team so corrective action can occur if necessary. This universal practice has been shown to limit complications and optimize clinical outcomes for patients undergoing this procedure.[38][39] [Level 5] In the event of an infection, an infectious disease specialty pharmacist may be consulted to best target antimicrobial therapy.
Contraindications
Contraindications for central venous access are always relative and dependent on the urgency and alternative venous access. Site-specific contraindications include distorted local anatomy, skin infection overlying the insertion site, thrombus within the intended vein, or the presence of other indwelling intravascular hardware within the intended vessel. Coagulopathy and bleeding disorders are considered relative contraindications even when they are severe. A systematic review studying the risk of complications following CVL placement in patients with moderate-to-severe coagulopathy and thrombocytopenia revealed that the incidence of major bleeding complications is low, and evidence supporting the correction of coagulopathy before CVL placement is lacking. [15] Ultrasound-guided placement of CVL is the method of choice in patients at high risk of bleeding due to underlying disorders of haemostasis, as it allows for safe and reliable access to central veins with low rates of complications and lesser attempts in patients with these disorders
Why measure the CVP line?
CVP is an indicator of right ventricular and, to a lesser extent, left ventricular preload. CVP also reflects the limit to venous return and informs about right ventricular function. As such, CVP measurements may be helpful to guide fluid management.
recorded at the end of expiration
measured by transducing the waveform of a central venous lineelectronic transducer placed & zeroed at the level of the RA (the “phlebostatic axis” – usually the 4th intercostal space in the mid-axillary line is used)
USES OF RAISED CVP
· Right ventricular failure
· Tricuspid stenosis or regurgitation
· Pericardial effusion or constrictive pericarditis
· Superior vena caval obstruction
· Fluid overload
· Hyperdynamic circulation
· High PEEP settings
What is the greatest risk for individuals with central venous access devices?
Infection. One of the most serious complications of VADs is infection, including bacterial endocarditis. Central devices, including PICCs, carry greater risk of infection because they are open to the larger veins of the body. Tunneled catheters have lower infection rates and ports risk even fewer infections
What are the risks and benefits of central line placement?
It makes blood draws easier and allows for the delivery of large amounts of fluid for medication or hydration. Some types of central lines can remain in place for weeks or even months. A central line is very useful. However, it's not without risks, including the potential for infection, a collapsed lung, and more.7 F
When inserting a catheter, one should use maximal sterile-barrier precautions, including a mask, a cap, a sterile gown, sterile gloves, and a large sterile drape. This approach has been shown to reduce the rate of catheter-related bloodstream infections and to save an estimated $167 per catheter inserted
How do you take care of a central line?
Preventing a Problem with a Central Line
1. Wash your hands before doing any central line care and wear gloves.
2. Always keep a clean and dry dressing over the central line site.
3. Follow the instructions for cleaning the cap and using sterile equipment.
4. Avoid tugs or pulls on the central line
5. What happens if central line is in right atrium?
6. What are the mechanical complications after central venous Catheterisation?
7. Major mechanical complications (major bleeding, arterial catheterisation, symptomatic arrhythmia, pneumothorax, and persistent nerve injury) typically require acute treatment or invasive intervention, in combination with prolonged observation of the patient.
What are the most common central line infections?
Coagulase-negative Staphylococci, Staphylococcus aureus, and Enterococcus are the most common organisms. Methicillin-resistant staphylococcus is frequently seen.
What is a common complication of central venous catheter?
The most common complications occurring during CVC application are: hearth arrhythmias, artery puncture, improper position of CVC and hematomas at the place of catheter insertion. If the top of the catheter enters the right hearth chambers, it can cause hearth arrhythmias by touching the hearth structures
The 5 Most Common Central Venous Catheter Complications
- Damage to central veins
- Pulmonary, or lung, complications
- Cardiac, or heart, complications
- Device dysfunction
- Infection
What is the most common complication of central line?
Vascular complications: The vascular complications seen during a central line insertion are arterial injury, venous injury, bleeding, and hematoma formation [14]. Ultrasound guidance has been shown to greatly reduce the risk of vascular complication
How long do you keep dressing on after central line removal?
Dressing
Care
The original dressing should be left in place for at least 48 hours, as long as it is not soiled or loose. If the dressing
becomes soiled or loose, it must be changed. After 48 hours, all dressings can
be removed if the site has scabbed underneath
What are the types of potential complications of a Central Line?
· Central Line-Associated Bloodstream Infection (CLABSI) ...
· Collapsed Lung (Pneumothorax) ...
· Delayed Pneumothorax (after 24 hours) ...
· Artery Puncture. ...
· Nerve or Vein injury. ...
· Blood Clot (Thrombus) ...
· Air Bubble in the Blood (Air Embolism) ...
· Irregular Heartbeat
Discussion
What are the nursing responsibilities for central line insertion?
What are the problems with central line insertion?
How can you prevent complications of central venous catheterization?
Discuss strategies to overcome infection occur for patients with CVP line?
REFERENCES