Intra- Operative Management and Nursing Care Using The Nursing Process
| Site: | Nilai Uni Connect |
| Course: | Perioperative Care; Fluid and Electrolyte |
| Book: | Intra- Operative Management and Nursing Care Using The Nursing Process |
| Printed by: | Guest user |
| Date: | Friday, 4 April 2025, 12:12 PM |
1. PHYSICAL ENVIRONMENT OF THE OPERATING ROOM

2. ZONING OF THE THEATRE COMPLEX
The surgical suite is a controlled environment designed to minimize the spread of pathogens and allow a smooth flow of patients, staff, and equipment needed to provide safe patient care. The suite is divided into three distinct areas: unrestricted, semi restricted, and restricted areas.
The OR is divided into 3 zones:
- unrestricted area
- semirestricted area
- restricted area
UNRESTRICTED AREA
The unrestricted area is where people in street clothes can interact with those in surgical attire. These areas typically include the points of entry for patients (e.g., holding area), staff (e.g., locker rooms), and information (e.g., nursing station or control desk).
UNRESTRICTED ZONE: Area outside the OR Complex.
Personnel is not in theatre attire (clean pants/top; footwear; cap; mask) Non OR staff / visitors can be in this area
SEMIRESTRICTED AREA
The semirestricted area includes the surrounding support areas and corridors. Only authorized staff are allowed access to the semirestricted areas. All staff in the semirestricted area must wear surgical attire and cover all head and facial hair.
SEMIRESTRICTED ZONE: The OR staff in theatre attire but no need for mask; but Outside personnel must change footwear before entering this zone. Pre-op patient waiting area (Reception)

RESTRICTED AREA
In the restricted area masks are required to supplement surgical attire. The restricted area can include the OR, scrub sink area, and clean core.
RESTRICTED ZONE: This area personnel full theatre attire there is positive pressure ventilation. Surgical procedure takes place here.

Traffic flow in the OR follows the Zoning concept:
UNRESTRICTED ZONE
^ V
SEMIRESTRICTED ZONE
^ V
RESTRICTED ZONE
STRUCTURAL COMPLIANCE
- TEMPERATURE: Keep bacterial count in 180C - 220C environment low
- AIR EXCHANGE:20 – 25 Air Exchanges per clean air in an hour; to maintain circulation
- AIR FLOW: From the top corner through a corner opposite in the lower end
Around the OR Table – Vertical Laminar flow, flowing from the top downwards and outwards.
POSITIVE PRESSURE
Highest pressure in the RESTRICTED ZONE VENTILATION
Lower pressure in the Semi restricted Zone but this pressure is higher than the Unrestricted Zone
FLOW OF AIR IS FROM RESTRICTED ZONE TO UNRESTRICTED ZONE
OTHER CONTROLS TO KEEP ENVIRONMENT SURGICALLY CLEAN:
- Personnel change to OR Attire
- Personnel with URTI / other infections not allowed to circulate/scrub for cases
- Cleaning Routine for OR Complex
- Beginning of the day
- Between Cases
- Terminal Cleaning at the end of the day; between cases, after biohazard cases
- Yearly Cleaning (Close theatre; High Dusting, Painting, Major Repairs, Equipment Check/Replacement)
- Controlled Movements by Personnel
- Sliding Doors
- Keeping Biohazard Cases last in the list
- Keep Orthopedic Implant Room Specific
- Spillage protocol
DESIGNATED AREAS IN THE OR
- Airlock
- Reception Area
- Scrub Room
- Operating Room where the intervention is done
- Instrument Preparation Room
- Sterile Pack Room
- Storage Room for Sterile Surgical Supplies
- Storage Room Non-Sterile Supplies
3. THE OPERATING ROOM

- OR Table
- PT Light
- Anesthetic Machine
- Monitors
- 2 Suction Machines
- Diathermy Machine
- X-ray viewer
- Drugs / I/V Solutions / Sutures
- Floor Bowls / Trolley/Mayo Table
4. THE OPERATING TEAM
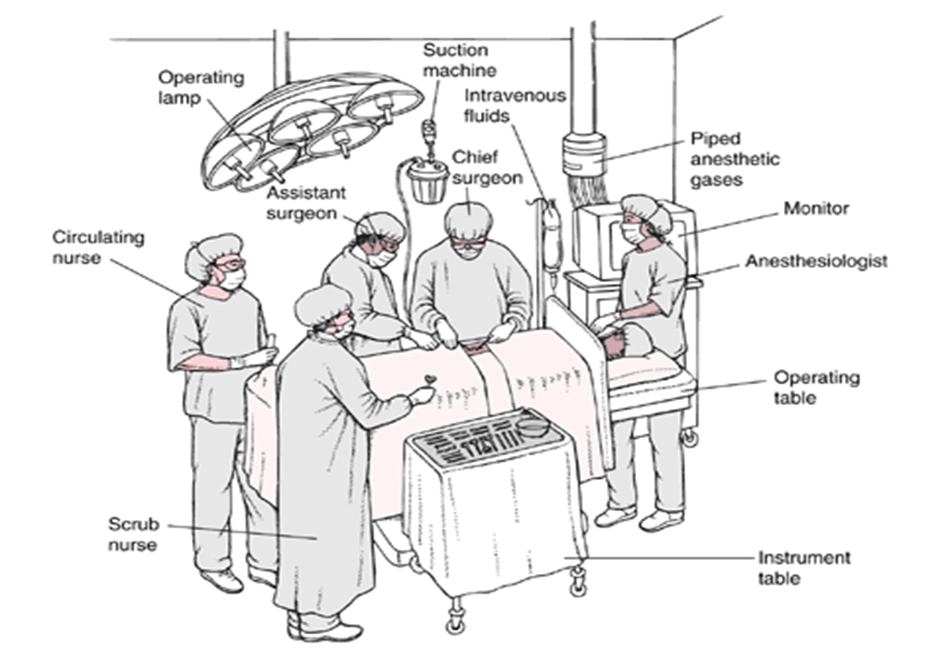
SURGICAL TEAM

Surgeon
Surgeon heads the surgical team together with assistants, scrubs and performs the surgery.
Anesthesiologist or Nurse Anesthetist
Anesthesiologist or nurse anesthetist, administers the anesthetic agent and monitors the patient’s physical status throughout the surgery.
Registered Nurse
The perioperative nurse is a registered nurse (RN) who implements patient care during the perioperative period. Through close collaboration with the other members of the surgical team, you prepare the OR for patients before they arrive. You are usually the first member of the surgical team who meets the patient. You are the patient’s advocate throughout the intraoperative experience. This includes maintaining the patient’s safety, privacy, dignity, and confidentiality; communicating with the patient; and providing physical care. Assess the patient to determine any additional needs or tasks to complete before surgery. Provide physical and emotional comfort and patient and caregiver teaching regarding the upcoming surgery. In addition, work with the patient’s caregivers, keeping them informed and answering questions. This is particularly important in day-surgery areas where caregivers must assume greater responsibility for preoperative and postoperative care.In the perioperative role, you assume functions that involve either sterile or unsterile activities.
Scrub Nurse
When you serve in the role of scrub nurse, you follow the designated scrub procedure, are gowned and gloved in sterile attire, and remain in the sterile field. include performing a surgical hand scrub setting up the sterile tables preparing sutures, ligatures and special equipment (such as a laparoscope); assisting the surgeon and the surgical assistants during the procedure by: anticipating the instruments that will be required.


Circulating Nurse
When you serve in the role of circulating nurse,or circulator you remain in the unsterile field and so you are not gowned and gloved in sterile attire.Other task are:
- He or she manages the operating room protects the patient’s safety and health by monitoring the activities of the surgical team checking the operating room condition continually assessing the patient for signs of injury.
- Assisting with patient positioning.
- Preparing the patient’s skin for surgery.
- Managing surgical specimens, and documenting intraoperative events.

5. INTRAOPERATIVE NURSING CARE
Intraoperative nursing phase begins when the patient arrives in the surgery and anesthesia unit for their operation. Nursing in the operation room setting is typically very intensive and systematic. Patient should be cared for from a holistic perspective, both physical and emotional needs taken care of.
Surgical asepsis: Ensure sterility Alert for breaks –surgical conscience.
Surgical conscience: The awareness, which develops from a knowledge base, of the importance of strict adherence to principles of aseptic and sterile techniques.

6. MANAGEMENT PATIENT DURING SURGERY
Room Preparation
Before transferring the patient into the OR, prepare the room to ensure privacy, prevention of infection, and safety. Individualization of this preparation is essential to achieve the expected patient outcomes. For example, when an obese patient is admitted to the OR, there are several special considerations Ask such questions as, What equipment is needed to safely transfer the patient to and from the OR table? Will extra staff be required for safe transfer and positioning? Is special equipment needed (e.g., extra-long instrumentation)? What special precautions, if any, must be taken to ensure maintenance of the patient’s airway? The unique needs of each patient must be addressed for a safe surgical experience.
Surgical attire (pants and shirts, masks, protective eyewear, and caps or hoods) is worn by all people entering the OR All electrical and mechanical equipment is checked for proper functioning. Aseptic technique is practiced as each surgical item is opened and placed on the instrument table. Sponges, needles, instruments, and small medical devices (e.g., surgical clip cartridges, universal adapters) are counted according to strict processes to ensure accurate retrieval at the end of the procedure. Any retained surgical supplies, devices, or instruments are sentinel events that can result in negative outcomes for the patient.

During room preparation and the surgical procedure, the scrub person performs surgical hand antisepsis, dons’ sterile gown and gloves, and touches only those items in the sterile field. The circulating nurse remains in the unsterile field and performs those activities that permit touching all unsterile items and the patient. This coordinated effort allows for smooth functioning throughout the procedure.
Transferring Patient
Once the patient’s identity has been verified and the OR has been prepared, the patient is transported into the room for the surgery. Each time a patient is transferred from one bed to another, the wheels of the stretcher must be locked, and a sufficient number of personnel should be available to lift, guide, and prevent accidental falling or injury to self, other staff, or the patient. Once the patient is on the OR bed, place safety straps snugly across the patient’s thighs. At this time the monitor leads (e.g., electrocardiogram [ECG] leads), BP cuff, and pulse oximeter are usually applied and an IV catheter is inserted if it was not done in the holding area.
Scrubbing, Gowning, and Gloving
Surgical hand antisepsis is required of all sterile members of the surgical team (scrub nurse, surgeon, and assistant). When the procedure of scrubbing is the chosen method for surgical hand antisepsis (often for the first case of the day), your fingers and hands should be scrubbed first with progression to the forearms and elbows. The hands should be held away from surgical attire and higher than the elbows at all times to prevent contamination from clothing or detergent suds and water from draining from the unclean area above the elbows to the clean and previously scrubbed areas of the hands and fingers.
Waterless, alcohol-based agents are replacing traditional soap and water in many facilities. When using an alcohol-based surgical hand-scrub product, prewash hands and forearms with soap and dry completely before applying the alcohol-based product. After application of the alcohol-based product, allow hands and forearms to dry thoroughly before donning sterile gloves.
Once surgical hand antisepsis is completed, the team members enter the OR to put on surgical gowns and two pairs of gloves to protect patients and themselves from the transmission of microorganisms. Because the gowns and gloves are sterile, those who have scrubbed can manipulate and organize all sterile items for use during the procedure.
Intraoperative nursing
Intraoperative nursing involves caring for patients from the time the patient enters the operating/procedure room, through the procedure, and until the patient is transferred to the post anesthesia care unit (PACU).